Pain and Pain Pathway
Definition of Pain
It is an unpleasant sensation created by a noxious stimulus that is mediated along specific nerve pathway into the central nervous system where it is interrupted as pain.
Dual Aspect of Pain
The transmission of the impulse and the interruption of and the reaction to the impulse demonstrate the dual aspect of pain.
Pain Perception
It is the physioanatomical process by which pain is received and transmitted, by the neural structures, from the end organs or pain receptors to the central nervous system.
This phase of pain is the same in most healthy persons, but it can be affected by diseases and toxic status. This phase needs an intact neural mechanism.
Pain Reaction
It is the patient’s manifestation of his perception of pain. This phase include extremely complex neuroanatomical and physio-psychological features. The patient’s reaction to pain differ from patient to patient and from time to time in the same patient. The degree of pain reaction is determined by the patient pain reaction threshold. Pain reaction threshold inversely proportionate with pain reaction. The higher the pain threshold the less is the pain reaction. Patients manifestation to pain include facial expressions, crying out, tapping feet, ect...
Pain reaction depends on the functioning of the thalamus and the cortex as follows:
- Depressed thalamic action result in increase in pain thresholds and greater tolerance to pain.
- Slight cortical depression, as with small doses of barbiturates result in a greater reaction to pain due to the removal of complete conscious control.
- Increased cortical depression may result in complete elimination of pain reaction by producing unconcsiousness and general anaesthesia.
Factors Affecting Pain Threshold
- Emotional Status: Patients who are emotionally unstable will have low pain reaction threshold and a greater pain reaction.
- Fatigue: Fatigued patients will have a lower pain reaction threshold and in turn a higher pain reaction.
- Age: Older patients tends to tolerate pain, and thus have higher pain reaction threshold than younger patients or children. This may be due to the realization that unpleasant experience is part of life. In case of senility the process of pain perception itself may be affected.
- Sex: It is generally accepted that males have higher pain reaction threshold than females. This may be a reflection of the male desire to maintain his feeling of superiority.
- Fear and Apprehension: Individuals who are apprehensive and extremely fearful of a procedure tends to magnify, within their minds, the unpleasant experience. This result in lowering the pain reaction threshold.
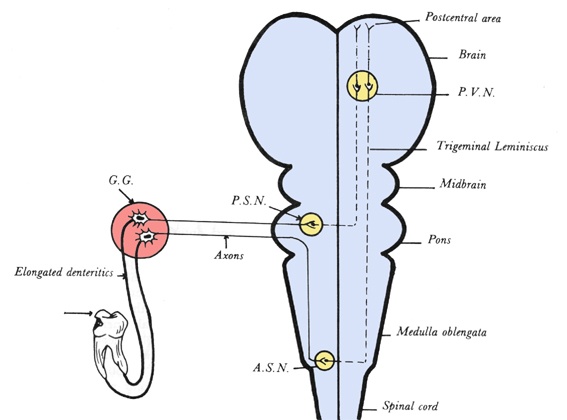
Pain Pathway
The stimulus is first received by both the myelinated and unmyelinated fibers of the trigeminal nerve, which is the principal sensory nerve of the head region. The stimulus is then conducted as an impulse along the afferent fibers to the semilunar or gasserian ganglion. The impulse is then mediated by the sensory root of the nerve into the pones. In the pones the sensory root either ends directly into the “Principle Sensory Nucleus” or bifurcate into ascending and descending fibers. The ascending fibers convey general tactile sensation while the descending fibers convey temperature and pain sensation. (Fig. 2-1) The pain impulse descends from the pones via the spinal tract fibers of the trigeminal nerve, through the medulla down to about the level of the second cervical vertebra where it enter the “Accessory Sensory Nucleus”
Axones of the second neuron emerges from the spinal nuclei, cross the midline and ascend to join the fibers of the mesencephalic nucleus to form the trigeminal leminscus or the spinothalamic tract. The spinothalamic tract continue upwards and terminate in the posterioventral nucleus (PVN) of the thalamus. On reaching the PVN the pain impulse is conveyed to the third neuron. Fibers of the third neuron projects from the PVN to the posterior central convolution of the posterior cortex where pain sensation is felt.
Methods Of Pain Control
As pain is divided into two phases, namely pain perception and pain reaction, methods of pain control affect either one of the two phases.
Removing the cause of pain
It is obvious that removing the cause of pain prevent the initiation of the painful impulse. If this could be accomplished the environmental changes in the tissue would be eliminated. Thus the free nerve endings would not be excited and no impulse would be initiated.
Blocking the pathway of the impulse
By this method a suitable drug possessing local analgesic properties is injected into the tissue in proximity to the nerve involved. The drug well prevent the depolarization of the nerve fibers at the are of absorption. In this way the drug will prevent the conduction of any impulse centrally beyond that point.
Raising the pain threshold
This method utilizing the use of certain drugs that have analgesic properties which result in raising the pain threshold centrally and thus interfere with the pain reaction phase. Drugs possessing analgesic properties and can be used in controlling pain include acetylsalicylic acid which is effective against mild pain and narcotics and morphine which are effective against sever pain. However many of these drugs have undesirable side effect especially with prolonged use, e.g. addiction which may develope with the prolonged use of morphine.
Preventing pain reaction by cortical depression
Eliminating pain by this method is within the scope of general anaesthesia. The anaesthetic agent by its increasing depression of the central nervous system prevents any conscious reaction to a painful stimuli.
Using psychosomatic method
This method depends for its effectiveness on putting the patient in proper frame of mind. One of the most important factors in this method is the honesty and sincerity toward the patient. This necessitates keeping the patient well informed about the procedure and what he might expect. Always keep in mind that the central nervous system dislike surprises and may react quite violently to any unpleasant surprise.
Regional Anaesthesia "General Consideration"
Definitions
Regional analgesia is the loss of pain sensation over an area of the anatomy without loss of consciousness. Regional anaesthesia, on the other hand, is loss of pain and other sensation, as temperature, pressure and motor function, over an area of the anatomy without loss of consciousness.
The two terms, analgesia and anaesthesia, are often used interchangeably. However, each term indicate different action of the drug,.
Indications Of Local Anaesthesia
Generally local anaesthesia is used whenever it is necessary for the patient to remain conscious while insensibility to pain is produced over an area or teeth. Local anaesthesia is indicated in the following cases:
- Extraction and surgical removal of teeth.
- Intraoral surgical procedures.
- Operative work.
- Endodontic work.
- As a diagnostic method for vague pain in and around the face and neck.
Contraindication Of Local Analgesia
- The patient refuse local anaesthesia because of fear and apprehension.
- The presence of infection in the pathway of the needle.
- If the patient is allergic to various local anaesthetic agents.
- In very young patients below the age of reason.
- Uncooperative patients due to mental disturbances or epilepsy or other conditions.
- In cases of anatomical anomalies which make injection of local anaesthesia difficult or impossible.
- If major surgery is to be performed.
Factors Which Govern Maximum Effect Of Local Anaesthesia
Distance of the nerve in contact with the drug: The local anaesthetic drug must come in contact with at least 8-10 mm. of the nerve, to block 2-3 nodes of Ranvier. If a shorter length is affected the analgesia will be incomplete.
The size of the nerve fibers: The larger the fibers the more difficult to be anaesthetized as they are less easily affected by the drug and thus require a greater concentration. This may be due to the larger surface area of the nerve in relation to the volume of the drug.
Drug concentration: When inadequate concentration is used the block may be incomplete. This is manifested by the patient being insensitive to a single stimulus but responsive to repeated stimuli.
Methods Of Conduction Of Regional Analgesia
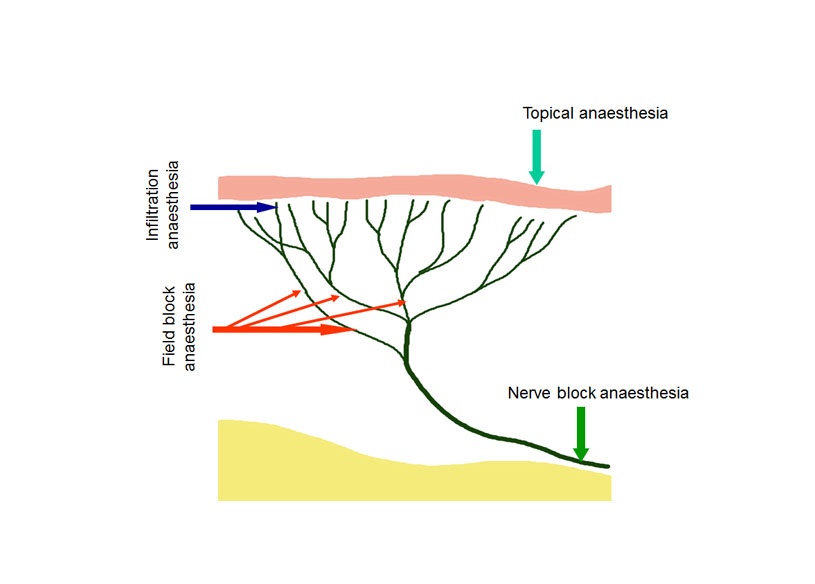
I. Topical Analgesia
In this method the free nerve endings, in an accessible structures as the skin and mucous membrane, are rendered incapable of stimulation by applying chemical ointment or solution which penetrates through the epithelium to reach the free nerve endings. This method is used for simple superficial procedures and to permit painless insertion of needles.
II. Infiltration Analgesia
In this method the free nerve endings are flooded by the injectable anesthetic solution thus rendering them incapable of being stimulated. There are two types of infiltration anaesthesia, bony tissue and soft tissue infiltration.
A. Bony tissue infiltration
This method is also called “Intraosseous infiltration”. In this method the cortical bony plate is penetrated and the anaesthetic solution and the anesthetic solution is injected into the spongy bone. Thus the terminal nerve endings in the area are anaesthetized.
A pathway should be made through the mucoperiosteum and the bone using a suitable instrument, usually a bur, through which the needle is passed to the spongy bone. Also a special strong needle may be used.
B. Soft tissue infiltration
Submucosal infiltration: The needle is inserted beneath the mucosal layer and solution is deposited.
Paraperiosteal infiltration: The needle is inserted till it contacts the periosteum. This is known by feeling resistance in the pathway of the needle. No force should be made to force the needle further toward the bone otherwise the needle may be broken or bend. As the solution is injected it will diffuse through the periosteum and the bone to reach the free nerve endings in the spongy bone. No trial should be made to inject the solution subperiosteal as it has the following disadvantages:
- Liability of needle brokage.
- Difficulty of forcing the solution between the periosteum and the bone, in addition to the sever pain when the solution strip the periosteum from the bone surface.
Field Block Infiltration: In this method the anaesthetic solution is deposited in proximity to the larger terminal nerve branches. Accordingly, the area to be anaesthetized is walled off to prevent the passage of afferent impulses.
III. Nerve Block Analgesia
In this method the anaesthetic solution is deposited in close proximity to the main nerve trunk supplying the operative field before it divides into its terminal branches. In this way the afferent impulses will be prevented from travelling centrally behind that point.
Advantages Of Nerve Block Over Infiltration Analgesia
- Nerve block anaesthesia gives more profound anaesthesia of longer duration.
- Fewer needle punctures are needed which mean less psychic and puncture trauma to the patient.
- If infection is present, possibility of infection dissemination by the needle is eliminated as the injection is done at a distance from the infection site.
- It allows surgical work on large field with few volume of the anaesthetic solution, thus decrease the chance for development of drug toxicity.
- No local ischemic effect from the vasoconstrictor agent, which is added to the anaesthetic drug, thus decrease the possibility of infection which may result from the poor circulation to the surgical afield. In addition, good blood supply helps quicker healing and decrease postoperative pain.
Causes Of Failure Of Local Analgesia
Failure of local anaesthesia may be due to one or more of the following reasons:
- Improper technique of injection.
- The use of too weak concentration or too small volume of the anaesthetic drug.
- Injection into a blood vessels, thus the drug is quickly washed away from the area. In such case there is great possibility for development of toxicity.
- Escape of the analgesic solution into the weak facial planes in the area away from the region, thus no enough volume of the drug come in contact with the nerve.
- The patient is resistant to the anaesthetic drug. However, the patient is usually resistant to one type of drugs but any other type would be affected.
- The presence of variation in the normal anatomy which leads to improper injection technique.
- The presence of acidity in the field of injection. (See explanation Page 50)
Factors Governing The Selection Of The Method Of Induction
Area to be anaesthetized
When a single tooth or a small area is to be anaesthetized a complicated extraoral nerve block is unnecessary. Also when field block is sufficient, nerve block is undesirable, i.e. the simplest method is the best.
Infiltration anaesthesia depends largely, when a tooth is to be anaesthetized, on the diffusion of the solution through the cortical plate of bone to reach the nerve filaments in the cancellous bone. So it is only successful in regions where the cortical plate is thin or of reasonable thickness.
Duration and profoundness required
Certain methods have longer duration and give more profound anaesthesia. Accordingly if the expected operating time is relatively long nerve block is more suitable.
Extent of the surgical procedure
In cases of multiple extraction or working on a large operative field, nerve block is indicated to avoid multiple needle punctures and the use of too large volume of the anaesthetic solution if infiltration technique is used.
Age and condition of the patient
Old patients has a dense impenetrable bone while children reacts adversely to extensive anaesthetic areas and the uncomfortable feeling of numbness. Accordingly, nerve block technique is suitable with old age and infiltration techniques are suitable with young patients.
The general condition of the patient should be taken into consideration as in some cases any pain may be harmful, as in patients with angina pectoris where pain may precipitate the attack. Thus any method offering more profound anaesthesia would be desirable.
Haemostasis, if needed
The vasoconstrictor used with the anaesthetic solution reduces greatly the amount of blood oozing in the field of surgery but only when injected in the area. Therefore, when bloodless field is needed infiltration anaesthesia is to be used.
The presence of infection
Injection in an infected area may cause spreading of the infection. In addition the effectiveness of the anaesthetic drug will be greatly reduced. Obviously infiltration anaesthesia should be avoided in such cases.
Skill of the operator
The skill of the operator to perform the technique of injection properly should be taken into consideration.
Local Anaesthetic Drugs
Local analgesic drugs can be defined as those drugs that have little or no irritating effect when injected into the tissues and that will temporary interrupt conduction when absorbed into the nerve. Blockage of nerve fibers which transmit pain sensation will result in regional analgesia.
These local analgesic agents are all synthetic compounds, with exception of cocaine which is seldom used today. The modification of the cocaine molecule has been responsible for the production of a large number of local analgesic agents that have a definite relationship between their chemical structure and their analgesic properties.
Properties Of An Ideal Analgesic Agent
- It should have a reversible action.
- When injected it should be nonirritating to the tissue and produce no secondary local reaction
- Produce no systemic toxicity.
- Have rapid onset and sufficient duration.
- Potent enough to allow the use of non toxic concentration.
- Have sufficient penetrating properties to be used as topical analgesic.
- Stable in solution and undergo biotransformation readily in the body.
- Produce no allergic reaction.
- Can be sterilized without deterioration.
Unfortunately non of the available agents fulfill all these properties, particularly as regard duration, toxicity and potency.
Common Properties Of The Injectable Local Analgesic Agents
- All are synthetic compounds that contain amine group.
- All form salts with strong acids which is water soluble.
- Alkali will hydrolyze the salt to free the alkaloid base which is soluble in lipids.
- When injected in the body they are either hydrolyzed by plasma proteins or undergo biotransformation in the liver.
- All affect the nerve conduction in a similar manner and have a reversible action.
- All are compatible with epinephrine and other vasoconstrictors.
- All are not or slightly irritant to the tissue in the concentration used.
- All are capable of producing toxic effect when sufficient high plasma concentration is reached.
Table 1. Injectable local analgesics.
I. Ester Group
A. Benzoic Acid Esters
- Piperocaine (Metycaine)
- Meprylcaine (Oracaine)
- Isubocaine (Kincaine)
B. Para-Amino Benzoic Acid Esters
- Procaine (Novocaine)
- Tetracine (Pontocaine)
- Butethamine (Monocaine)
- Propoxycaine (Ravocaine)
- Chloroprocaine (Nesacine)
C. Meta-Amino Benzoic Acid Esters
- Metabutethamine (Unacaine)
- Primacaine
D- Paraethoxybenzoic Acid Esters
- Paraethoxcaine (Intracaine)
E- Cyclohexylamino-2 Propyl-Benzoate
- Hexylcaine (Cyclcaine)
II. Non-Ester Group
- Lidocaine (Xylocaine)
- Mepivacaine (Carbocaine)
- Pyrrocaine ( Dynacaine)
- Prilocaine (Citanest
Classification Of Local Analgesics Used
The local analgesic drugs used in dentistry are divided into three groups, the ester group, the amide group and the hydroxy group.
I. Ester Group
It is composed of an aromatic group, an intermediate chain containing an ester linkage and a hydrophilic secondary or tertiary amino group which forms water soluble salts when combined with acids.
II. Amide Group
It is composed of an aromatic lipophilic group, an intermediate chain containing amide linkage and a hydrophilic secondary or tertiary amino group which forms water soluble salts when combined with acids.
III. Hydroxy Group
They are almost insoluble in water as they lack the hydrophilic portion. They are used as topical analgesics.
The local analgesics can be grouped according to their chemical structures. This is important as regard their biotransformation as well as the possibility of allergic reaction. Patient who is allergic to any one drug is usually allergic to any other drug of the same or closely related chemical structures. Table I shows a list for the available injectable local analgesics.
It should be mentioned here that the injectable synthetic local analgesics are so balanced chemically that they have both lipophilic and hydrophilic properties. If the hydrophilic property predominates the free base will not be radially precipitated after injection and the ability oft he drug to diffuse through the lipid rich nerves decrease. On the other hand, if the lipophilic property predominates the drug will be insoluble in water and unable to diffuse through the interstitial tissues.
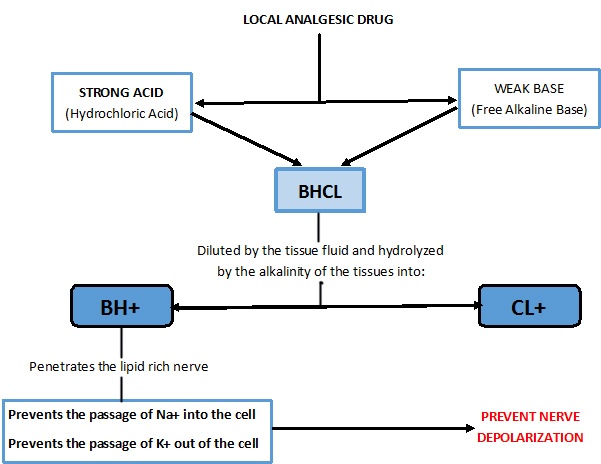
Mode Of Action Of Local Analgesics
The local analgesic drugs, by an unknown action on the minute openings in the nerve membrane, prevents the passage of Na+ into the cell and the passage of K+ out of the nerve cell. Thus the polarized nerve is unable to depolarize and conduct an impulse. The prevention of depolarization must take place over a length of two or three nodes of Ranvier as the drug reaches the myelinated nerve at these sites. Figure 2 shows a scheme which summarize the mode of action of the local analgesic agents.
Factors Affecting The Action Of Local Analgesics
1. Alkalinity
Alkalinity of the tissues will affect the ionization of the drug and the rate of liberation of the free base. The local analgesic drug is present in the tissue in two forms, the ionized and unionized forms. Ionization depends on the ionization constant of the drug and the pH of the tissues. The higher is the ionization constant of the drug, the less is ionization and the less is the pH of the tissue (more acidic) the less is ionized form.
Pus has an acidic pH and it interfere with the development of potent analgesia preventing the release of the free base and retardation of ionization of the free base.
2. Lipid solubility
As the diffusion of the free base into the nerve fibers depends on its lipid solubility, the potency of the local analgesic drug is in direct proportion to its lipid solubility.
3. Type and size of the nerve
The myelinated nerves require more concentration and time to be blocked than the unmyelinated nerves. This is because they are protected by an insulating barrier which is the myelin sheath. They are accessible to the drug only at the nodes of Ranvier.
On the other hand, the larger the diameter of the nerve the greater is the concentration required to block it. Pain and temperature fibers being smaller in diameter are blocked before the touch, proprioceptive and motor fibers.
4. Concentration of the drug
For effective local analgesia certain minimal concentration of the free base must be absorbed into the nerve fiber. The degree of analgesia depends not on the concentration of the drug injected but on the concentration of the free base which come in contact with the nerve fibers. There are many factors that may interfere with the development of adequate concentration of the free base in the nerve fibers, these are:
- Excessive alkalinity: Increased alkalinity causes precipitation of the free base before the solution, which is water soluble, diffuse toward the nerve. Thus absorption takes place before the free base, which is lipid soluble, comes in contact with the nerve fiber.
- Excessive dilution with blood or tissue fluids: Once the solution is injected the intercellular fluids immediately begins to dilute it. The molecules diffuse in all directions with the concentration decreasing as the solution leaves the original site of injection. Accordingly the greater the distance of the injection from the target nerve the lower is the concentration that reach the nerve.
- Too rapid absorption: An analgesic solution injected in a highly vascular area will be rapidly absorbed into the systemic circulation. The effective concentration outside the nerve will reduced. Also rapid absorption increases the possibility of development of systemic toxicity. Since most of the analgesic drugs are vasodilators the addition of a vasoconstrictor is advisable not only to prolong the duration of analgesia but also to decrease the possibility of development of systemic toxicity.
- Low alkalinity: As in cases of infection the alkalinity of the tissue is decreased to such an extent that the liberation of the free base and its ionization is inhibited.
Biotransformation Of The Local Analgesic Drugs
Injectable local analgesics undergo biotransformation according to their intermediate linkage group in the liver and the plasma. Ester group undergo biotransformation in the liver and the plasma while Amid group undergo biotransformation mainly in the liver. The enzymes responsible for biotransformation are the esterase enzyme in the liver and cholinesterase enzyme in the plasma.
Injectable Local Analgesic Drugs
I. Procaine (Novocaine)
Procaine is a relatively weak analgesic agent which have a low degree of toxicity. However, it is potent enough to produce safe and sure analgesia under almost all circumstances.
The drug is vasodilator so it is rapidly absorbed into the systemic circulation. Accordingly, addition of a vasoconstrictor is advisable. The drug is used in dentistry in 2% solution which has a sufficient potency and low systemic toxicity.
Pharmacological effect
- On central nervous system: It is capable of both stimulation and depression. The stimulation is usually an early response and may be manifested by excitement, tremors, ataxia (failure to regulate body poutsure and direction of limb movements) and even convulsion. Stimulation is usually followed by depression. It appears the initial excitatory effect is produced by inhibition of the cortical inhibitory neurons thus the facilatory pathway acts unopposed. With the increase of the drug dose inhibition of both the inhibitory and facilatory?? neurons occur resulting in generalized CNS depression. On the peripheral nerves the effect of all esters compound is always depression.
- On cardiovascular system: In the small doses used in dentistry the drug has no effect other than the vasodilatation of the vessels in the area. Systemically the drug cause depression of cardiac muscle, as well as smooth and skeletal muscles. In large doses the drug may produce hypotension by relaxation of the smooth muscles which result in generalized vasodilatation.
- On respiratory system: Large doses may severely depress respiration. In most instances of toxic over dose respiratory arrest occur before cardiac arrest.
II. Tetracaine (Pontacaine)
In equal concentration tetracaine is at least 10 times more potent and toxic than procaine. It is used in 0.15% solution which make it of equal toxicity to procaine. It is a potent topical analgesic which have a slow onset due to its slow rate of absorption. The drug cause no vasodilatation and has a duration of about 30-45 minutes.
III. Monocaine
This drug is 1.5 - 2 times more potent than procaine and only slightly more toxic. Onset is more rapid than procaine and has more diffusible rate. It used in dentistry in 1.5% and 2% concentrations. Duration, when used with adrenaline is 60-70 minutes for 1.5 concentration and 90-120 minutes for 2% concentration. The drug has systemic toxicity similar to that of procaine and posses no vasodilatation property.
IV. Nesacaine
The drug is a satisfactory short acting analgesic of low toxicity an extremely rapid onset. It is hydrolyzed in the plasma 4-5 times faster than procaine and less toxic. It is used in 2% solution and due to its short duration addition of vasoconstrictor is a must.
V. Unacaine
It is a rapid acting local analgesic agent that is twice as potent as procaine and is less toxic. It is non irritant when injected into the tissue and diffuse rapidly into the lipid rich nerves and has a mild vasodilator property. It is used in a concentration of 3.8%.
VI. Oxylocaine (Lidocaine)
This drug has a rapid onset and diffuses radially through the tissue and the lipid rich nerves. The drug has an excellent topical analgesic property when used in 4% or 10% concentrations.
Pharmacology
- Effect on the central nervous system: The drug depresses the CNS both centrally and peripherally. Convulsions may occur but it is believed to be due to depression of some areas in the brain rather than direct stimulation.
- Effect on cardiovascular system: Like all other local analgesic agents the drug produces an increase in the excitability threshold and the refractory period of the heart.
- Effect on respiratory system: Small doses of the drug has no effect on the respiratory system, but large doses may cause respiratory arrest and apnea which is the most common cause of death in case of systemic toxicity.
Biotransformation
Unlike ester group, anilide group undergo biotransformation in the liver rather than in the plasma. Accordingly this drug is to be used in cases of plasma cholinesterase deficiency and is contraindicated in cases of sever liver diseases. The by-products are excreted in kidneys.
VII. Citanest (Prilocaine)
The drug is used in 4% concentration either alone or with adrenaline. It is less toxic than oxylocaine and undergo biotransformation more rapidly.
Dosage
Dosage suggested for different local analgesic agents are always in the conservative side. This is to offer the dentist a wide range of safety taking into consideration that the office patients are ambulatory patients and expected to leave the clinic unassisted and have no side effects.
When deciding the dose the following should be taken into consideration:
- Age and general condition of the patients: The dosage mentioned on the pamphlet of the drug is usually for healthy adult patients. The age and any present systemic disease may alter the dosage.
- The vasoconstrictors: The vasoconstrictors used are in most cases the deciding factor when calculating the dosage. In most case the limit of the local analgesic volume that can be injected is guided by the vasoconstrictor dosage.
The local analgesic agents can be grouped according to their duration into:
- Short acting: Which have a duration of 45 - 75 minutes.
- Medium acting: Which have a duration of 90 - 150 minutes.
- Long acting: Which have a duration longer than 150 minutes.
Constituents Of The Local Analgesic Carpoule
The analgesic Carpoule contain substances other than the local analgesic drug. These substances are added to potentiate and to preserve the constituents of the Carpoule. It contains the following substances:
- The analgesic drug.
- A vasoconstrictor.
- Preservative substance.
- Vehicle to make the solution isotonic.
I. The analgesic drug
This is the main substance contained in the analgesic Carpoule.
II. The Vasoconstrictor
Adrenaline or other synthetic vasoconstrictors are added to the analgesic Carpoule to potentiate their action and prolong their duration. The vasoconstrictors cause local vasoconstriction of the vessels in the injected area, thus decrease the rate of absorption of the drug into the systemic circulation. (See Page ---)
III. Preservative
Sodium meta bisulfite is added, in a concentration of 0.5 mg/ml, to prevent oxidation of the vasoconstrictor and hence deterioration of the solution. Other preservative substance that may be used is methylparaben. It should be known that some individuals are sensitive to the preservative substance. Those patients should not take local analgesic solution that contain this substance.
IV. Vehicle to make the solution isotonic
Physiologic salt solution in the form of 0.9% sodium choleroid or Ringer’s solution which contain sodium chloride, calcium chloride and potassium chloride, are used as a vehicle to dissolve the analgesic drugs and other constituents of the solution.
The solution should be isotonic for maximum effect of the local analgesic agent. The use of hypotonic solution will result in the passage of the water from the intercellular fluid into the cell, while the use of hypertonic solution will result in the passage of the water from the cell to the intercellular fluids. In both situation the diffusion of the solution into the tissue and its effect on the nerve will be adversely affected.
The Vasoconstrictors
The vasoconstrictor is an integral and necessary part of the local analgesic solution used in dentistry. The vasoconstrictors used in dentistry are all sympathomimetic amines. They are unstable in solution, therefore it is a must to include a preservative in the local analgesic solution to prevent their oxidation.
The preservative commonly used is sodium meta bisulfite which compete with the vasoconstrictor for the oxygen available in the carpoule. Being more active the sodium bisulfite is oxidized to sodium bisulfate and the vasoconstrictor remains relatively stable.
Advantages
The presence of the vasoconstrictor in the analgesic solution offers the following advantages:
- Retard the absorption of the solution into the systemic circulation which allow the use of smaller volume of the solution, decrease the chance for development of systemic toxicity and prolong the duration of analgesia.
- It produces haemostasis in the operative field but only when infiltration analgesia is used.
- It increases the efficiency of the local analgesic drug.
This advantages of the vasoconstrictors are so interrelated that when one is gained others automatically follow.
Disadvantages
In dental practice most of the disadvantages that are attributed to the vasoconstrictors are mainly due to its practical abuse. These may be in the following ways:
- Too much volume, than what is actually needed, is used.
- Repeated injections increases the volume to nearly toxic level.
- Intravascular injection which result in toxic manifestations.
Mode of action and pharmacological effect
The vasoconstrictors are sympathomimetic in nature producing their effect by stimulating the adrenergic constrictors (alfa receptors) present in the site of injection. Most vasoconstrictors undergo rapid biotransformation in the blood stream, thus they are usually short acting. In small doses, like those used in dentistry, no other organs should be greatly affected. However, the use of large volume, high concentration or intravascular injection of even a small amount may result in toxic manifestations.
The Vasoconstrictor In Use
I. Epinephrine (Adrenaline)
It is the most potent and efficient vasoconstrictor used in dentistry. It has a short duration as it undergo rapid biotransformation in the blood. It may produce undesirable systemic effect in the form of tachycardia, headache and hypertension in some patients. It is used in a concentration of 1/100.000 and 1/50.000. Other concentrations are also available.
II. Norepinephrine
It is slimier to epinephrine but is less potent. Concentration used in dentistry is 1/30.000.
III. Nordefrin (Corbasil)
It is similar to epinephrine in almost all aspects. It is only 1/5 the potency of epinephrine. It is used in dentistry in a concentration of 1/10.000.
IV. Phenylephrine
It is the most stable and the weakest vasoconstrictor. It is used in a concentration of 1/2500.
Table 2 shows the relative potency and the maximum total dose of the vasoconstrictors.
Topical Analgesic Agents
The topical analgesia has many uses in dentistry which ranges from mild generalized desensitization of the oral cavity prior to impression taking to localized numbing of the mucosa before incision of an abscess. Generally, topical analgesia may be used in dentistry for the following procedures:
- Prior to injection to decrease the pain caused by the needle puncture.
- For minor surgical procedures as removal of very loose deciduous teeth or removal of very superficial sequestra.
- For incision of an abscess as infiltration analgesia is contraindicated because of the presence of infection.
- For deep scaling as it is sometimes quite painful.
Methods of application
- In mouthwashes.
- In lozenges.
- In pastes.
- In the form of spray.
- By refrigeration.
Classification
Topical analgesics can be divided into two groups:
- Topical analgesics that produce their effect by means of refrigerant action. Among this group is the topical used of ethyl chloride spray. Being volatile, ethyl chloride when sprayed on the era will evaporate. As it evaporates it causes drop in the temperature of the sprayed area which result in surface analgesia. Ethyl chloride is highly irritant and care when using it should be taken to protect the eyes.
- Topical analgesics that produce their effect by the action of chemical compound that is absorbed and diffuses from the surface of the skin or mucous membrane to reach the free nerve endings. This group of topical analgesics include Xylocaine 5%, Pontocaine 2% and Benzocaine 10-15%.