ANATOMY OF SALIVARY GLANDS
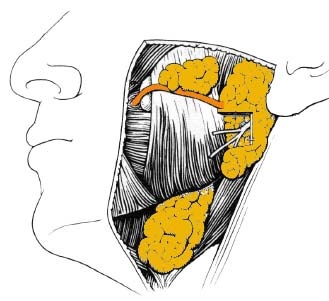
THE PAROTID GLAND
The parotid gland is the largest salivary glands. It lies below the external acoustic meatus and between mastoid process behind and ramus of the mandible in front. Anteriorly it overlaps the posterior part of the masseter. It extends downwards on the stylomastoid muscle. It is enclosed between two layers of cervical fascia, the parotid fascia.
The deep surface of the parotid is irregular and grooved obliquely by the styloid process and its attached muscles. Behind this process a lobe passes medially lying on the internal jugular vein and glossopharyngeal, vagus and accessory nerves. In front of the styloid process a large lobe, the carotid lobe, overlies the internal carotid artery and lies medial to the ramus and medial pterygoid muscle.
The accessory parotid gland is a separate lobe projecting from the anterior border and lying on the masseter muscle.
The parotid duct: It is 5 cm long, comes off from the anterior border crosses the masseter and turns at right angle to pierce the buccinator muscle and the buccal mucous membrane. The duct open in the mouth at a papilla opposite the upper second molar.
Course of the duct is represented by the middle third of an imaginary line from the intertargic notch the middle of the upper lip. The transverse facial artery lies superficial to the duct and the buccal branch of facial nerve deep to it.
Structures pass through the gland: The gland is traversed by the external carotid artery, retromandibular or posterior facial vein – the artery is deep to the vein. Most superficial the branches of the facial nerve transverse the substance of the gland.
Nerve supply:
Parasympathetic nerve supply: The glossopharyngeal nerve through the lesser petrosal nerve to Otic ganglion. Post ganglionic branches join the auriculotemporal nerve and supply the gland.
Sympathetic nerve supply: Branches from plexus around the middle meningeal artery (cell bodies in superior cervical ganglion)
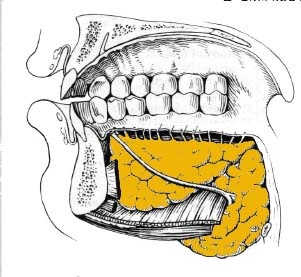
SUBMANDIBULAR GLAND
The gland lies in the submandibular fossa undercover of the body of the mandible in the submandibular triangle. The gland is divided into superficial and deep lobe.
Superficial lobe: Separated by stylomandibular ligament from the parotid gland. It is grooved above and behind by the facial artery. It lies on the mylohyoid, stylohyoid, hyoglssus muscles and anterior belly of digastric muscle. This lobe is covered superficially by the platysma muscle and cervical fasia and facial vein. It is bounded below by the tendon of diagastric nd related superficial to the submandibular lymph nodes which sometimes embedded into it.
Deep lobe: Passes with the duct between the mylohyoid and hyoglossus muscles arround the posterior free border of the mylohyoi muscle.
The submandibular duct: Passes with the deep lobe of the gland to the upper surface of the mylohyoid muscle. It has an intemiate relation with the lingual nerve throughout its course. At first the lingual nerve lies above the duct and the hypoglssal nerve below. The lingual nerve passes lateral to the duct then below to become medial to it. The duct passes upwards and forwards on the genioglossus muscle to open on papilla by the side of the lingual frenum.
Nerve supply:
Parasympathatic nerve supply: Reach the gland through the chorda tympani nerve synapsing in the submandibular ganglion.
Sympathatic nerve supply: From plexus arround facial artery.
SUBLINGUAL GLAND
The gland lies in the sublingual fossa of the mandible under mucous membrane of the floor of the mouth. The mylohyoid is inferior and the hyoglossus is medial to it.
Sublingual duct: The gland has about 18-20 ducts that opn separatly in the floor of the mouth.
Nerve Supply: as the submandibular gland.
MINOR SALIVARY GLANDS
Minor salivary glands are found in the mucosa of the lips, cheeks, palate and tongue.
EXAMINATION OF SALIVARY GLANDS
CLINICAL EXAMINATION
The initial step in the examination of the salivary glands should consits of face-to-face observation. Through this observation any signs of facial asymmetry, discoloration, visible pulsation or discharging sinuses can be observed. Figures 1 to 3 show the general anatomy of the major salivary glands.
Examination Of Parotid Gland
- Parotid enlargement: Enlargement of the parotid gland usually appears as a diffuse swelling, which when seen from the front, may left the lobule of the ear. The enlargement is more easily observed when it is unilaterally.
- Palpation: This is accomplished using the finger tips with a circular firm, but delicate, pressure over the gland (Fig 1). Any well defined nodule or diffuse swelling within the substance of the gland can be felt.
- Intraoral examination: Occasionally parotid tumors may grow in a parapharyngeal direction to occupy the lateral pharyngeal space. In such cases the tumor may be represented as a mass in the retromolar fossa.
- Parotid Duct (Stenson's duct): Using a lacrimal probe passed through the duct any obstruction or stricture can be detected.
- Nature of the flow: The gland is milked using extraoral pressure of the gland while observing the opening of the duct. Normally the gland excrete watery clear saliva. Diseased gland may excrete saliva containing purulent material, debris or thick mucous.
Examination Of Submandibular Gland
- Enlargement: Submandibular gland swelling may be diffuse or nodular. Swelling appears extraoral in the submandibular region. Diffuse swelling of the submandibular gland simply add fullness to the submandibular region.
- Palpation: Palpation of the submandibular gland is performed bimanually by placing the finger of one hand intraorally on the floor of the mouth and the fingers of the other hand are placed extraoral at the submandibular region and the gland is palpated between the two hands. (Fig. 4)
- Examination of submandibular duct (Warton's duct): The orifice of the duct can be locatd, at the floor of the mouth near the midline, by expressing saliva from the gland. A thin lacrimal probe is then inserted and advanced along the duct to detect any obstruction or stricture. (Fig 5-4)
- Nature of salivary flow: The gland can be milked by gentle firm pressure with one or two fingers placed just medial to the angle of the mandible and advanced forward. Normally the saliva should be viscous and clear.
Examination Of Sublingual Gland
Enlargement of the sublingual gland appears as an elevation in the floor of the mouth. The gland is palpated bimanually with one finger exerts pressure at the submental region and the other is placed intraorally.
Examination Of Minor Salivary Glands
Enlargement of minor salivary glands appears as discrete nodules within the substance of the submuscoa. Palpation of minor glands should be done bidigital when ever possible. This can be performed for examinning minor glands in the lips and cheek. Those of the palate are compressed aganist the bone of the hard palate.
RADIOGRAPHIC EXAMINATION
Plain Radiography
Plain films are suitable to demonstrate the presence of salivary calculi.
- Calculi situated in Wharton's duct are best demonstrated by intraoral occlusal film. On the other hand, calculi situated on the submandibular gland can be demonstrated by occlusal and/or extrtaoral films as lateral oblique view.
- Calculi on the parotid gland can be demonstrated by a periapical film held against the inside of the cheek while those situated on the substance of the parotid are demonstrated by extraoral films.
The calculi appears radiographically as a radiopaque object. Long standing stones may appear more radiopaque than the surrounding bone. However, some stone may have high organic content and appear more radiolucent. For this reason and in order not to burn-out these calculi, with high organic content, it is advisable to reduce the exposure time to 1/2 or 1/3 that used for dental and osseous structures.
Sialography
Sialography is a radiographic visualization of the ductal system of the gland. It is applicable for two of the three major salivary glands. the parotid and the submandibular glands. On the other hand, because of the multiductal nature of the sublingual salivary gland sialographic examination is not applicable for it. This visualization of the ductal system is made possible by the use of radiographic contrast solution introduced into the duct (Fig 5). Indication and contraindication of sialography are listed in table 1.
The contrast media is introduced into the gland by the aid of soft rubber catheters. Films are then taken to visualize the ductal system of the gland. Common views taken for parotid and submandibular glands sialography are listed in table 2.
There are wide variety of contrast media which can generally classified into water-soluble and fat-soluble. Ideal characteristics for sialographic contrast media are listed in table 3.
Table 1. Indications and contraindications for sialography.
Indications
1. To detect
- Calculi or foreign bodies within the gland or its duct.
- Ductal obstruction that is too small or poorly calcified stones that can not be detect by plain radiograph.
- Intraglandular neoplasms.
2. Useful in the following clinical situations
- Acute swelling of salivary glands, especially during eating. This situation is suggestive for an obstructive lesion as calculi or stricture or mucous impaction.
- Gradual progressive or chronic enlargement of the gland. Suggestive for chronic infection, benign tumors or malignant neplasms.
- The presence of a clinical palpable mass.
- Recurrent sialoadenitis.
- Dryness oft he mouth, to identify the cause.
- Pain of unknown origin.
3. Surgical considerations
- To determine the amount of damage to a gland.
- To indicate the proper site for a biopsy.
- To demonstrate an intrinsic or extrinsic mass and its site in the gland.
- To determine the relation of an intrinsic parotid mass to the facial nerve.
4. Therapeutic indication
- Dilatation of the ducatal system during the procedure may aid in the drainage of the ductal debris and removal of mucous plugs.
- Iodenated contrast medium is thought to have a bacteriostatic properties thatr may aid in sterilialization of the ductal system.
Contraindications
- Acute infection of the gland, as the ductal epithelium is disrupted and escape of the media may occur.
- In patients sensitive to the contrast media used.
- In cases of malignancies when clinical diagnosis is satisfactory.
Table 2. Common views taken for sialography.
Parotid Gland
- Antroposterior view.
- True lateral projection.
- Antroposterior view with the cheek in blow out position. For demonstration of the superficial portion of the duct and gland.
- Reverse basilar view to demonstrate the deep portion of the gland.
- Panoramic view.
Submandibular Gland
- Lateral oblique film.
- Panoramic view
- Occlusal intraoral film to demonstrate the duct of the gland.
Table 5-3. Ideal characteristics of sialographic contrast media.
- Physiologic properties similar to those of saliva.
- Absence of local or systemic toxicity.
- Pharmacological inertness.
- Satisfactory opacification.
- Low surface tension and low viscosity to allow filling of fine structures of the ductal system.
- Easy elimination but durable enough to allow time for satisfactory radiography.
- Residual contrast media that can be absorbed by the salivary gland and detoxified in the liver and excreted by the kindeny.
Technique
Sialographic technique can be divided into three phases. These are:
- Phase one: Preliminary films are taken to rule out the presence of obvious radiopaque pathosis.
- Phase two: The filling phase during which the contrast media is injected to outline the ductal system and, when necessary, the the glandular parenchyma. Films taken at this phase have great value in the study of mass lesions and obstructive lesions.
- Phase three: Films taken at phase three (evacuation and post evacuation phase) have little value in the study of mass lesions. Delayed or incomplete evacuation of the contrast media may be indicative for parenchymal destruction as in cases of chronic infection, irradiation or replacement by tumor.
Interpretation
- Sialolithiasis: Nonopaque stones will be demonstrated as a filling defects in the salivary gland duct. An air bubbles may be introduced into the canal during injection of the contrast media and may simulate a radiolucent stone. However, air bubbles are more mobile and may disappear or change position on subsequent films.
- Sialadenitis: This is inflammation of the gland that mainly involving the acinoparenchyme. In the filling phase the sialograph show the characteristic "apple tree in blossom" which is due to saccular dilatation of the acini and terminal ducts. In the evacuation phase the elimination of the contrast media is delayed. (Fig. 6)
- Salivary tumors: Sialograph help to determine the size and location of the tumor and its origin, whether intrinsic or extrinsic. (Fig. 7 and 8)
Computed Tomography (CT)
Computed tomography (CT) is the method of choice for examination of masses in and about the slaivary glands. The preesence or absence of a mass, its extent and whether it originate from within or outside the salivary gland can all be determined by CT examination. (Table 4 and Fig. 9)
Table 4. Role of computed tomography in diagnosis of salivary glands disorders.
- Determine the presence of a mass, its size, extent and origin.
- Determine whether a mass is circumscribed or invasive.
- Gives some indication about the histological nature of the mass, e.g. lipoma and cyst.
- Has limited role in examination of calculi and obstructive lesions as well as inflammatory conditions.
- Gives no information about the glandular secretory function.
Magnetic Resonance Imaging (MRI)
MRI is also used for diagnosis of salivary glands disorders. Although MRI is equal to CT as a diagnostic aid for salivary glands tumors yet it is superior to it in determining vascular tumors involving the salivary glands especially the parotid gland.
Radioisotpe Scans
The radioisotope examination is useful for evluationof the glandular parenchyma. The technique involve intravenous injection of a radioactive isotope (Technetium 99m) and examining the glandular uptake and evacuation of the isotope over a period of about 60 minutes. (Fig. 10)
Ultrasonography
Ultrasound echogram is useful in detecting space occupying lesions as well as differentiation between cystic lesions and solid mass lesions. A fluid filled space as cyst appears echo-free while solid structure appears filled with multiple echoes and various shades of grays (Fig. 11) However, sonography is not able to visualize the deep lobe of the parotid as it lies medial to the ascending ramus of the mandible.
BIOPSY OF SALIVARY GLANDS
Incisional biopsy for the major salivary glands, especially the parotid, is rarely undertaken unless the lesion is superficial and malignancy is suspected and can not be assured by other methods. Biopsy of major salivary glands should be avoided when ever possible because of the following:
- The close relation of the lesion to important structures, e.g. the facial nerve in case of parotid tumor.
- The possibility of creation of salivary fistula as repaire of the biopsy site is usually difficult especially in the presence of malignancy.
- The possibility of seeding neoplastic cells outside the gland.
On the other hand, minor salivary glands biopsy is undertaken for either removal of pathological tissues or for microscopic diagnosis of some diseases as Sjogren's syndrome and sarcoidosis. Sjogeren's syndrome is a condition characterized by dryness of the mouth due to wasting of the salivary glands that is associated with rheumatoid arthritis and dryness of the eyes. Sarcoidosis, on the other hand, is a chronic disorder of unknown etiology in which the lymph nodes in many parts of the body are enlarged and small granulomas develop in the lungs, liver and spleen. Salivary glands are also commonly affected. The most common suggested procedure for biopsy of the minor salivary glands is the removal of minor glands in the lower lip.
Fine Needle Aspiration Biopsy (FNAB)
Fine needle aspiration biopsy (FNAB) has become an acceptable practical and useful technique in the diagnosis of head and neck masses. The technique is simple and rapid and need no expensive instruments. The procedure can be performed on out patients basis using a 10-20 ml syringe and a 22-gauge needle. Smears are prepared for rapid cytological diagnosis (Fig. 12). The main reasons for performing FNAB is to answer the following questions:
- Is the mass originating from the salivary gland or from other tissue?
- Is the mass benign or malignant.
- Whether or not further investigations are necessary?
Aspiration biopsy results in accurate diagnosis in 90% of mixed tumors which are the most common tumors of the salivary glands. The major limitation of FNAB is the inability to examine some aspirates due to lack of suitable cellular materials and the need for an expert cytologist for the accurate interpretation.